At Texas Breast Center, under the expert care of Dr. Gorman, we understand the complexities that come with a breast cancer diagnosis, including the risk of lymphedema. Breast cancer management is a multifaceted approach that addresses various complications such as lymphedema. Lymphedema, a condition of localized fluid retention and tissue swelling, can be a challenging aspect of breast cancer care. Lymphedema occurs due to the disruption of the lymphatic system, which affects lymph vessels and lymph nodes. Our team is dedicated to providing clear, straightforward information to help you manage and prevent this condition. In this article, we’ll address common questions about lymphedema and its connection to breast cancer. If you have concerns or need personalized advice, schedule an appointment with Texas Breast Center for a consultation today.
How common is lymphedema in breast cancer?
Lymphedema is a common complication following breast cancer treatment. Research indicates varying prevalence and incidence rates, with studies showing that around 30% of women treated for breast cancer experience lymphedema. Specifically, the prevalence can increase from 6.8% at baseline to nearly 24% at seven years post-diagnosis. Cumulative incidence rates reveal that lymphedema affects about 13.5% of patients at two years, 30.2% at five years, and 41.1% at ten years post-treatment.
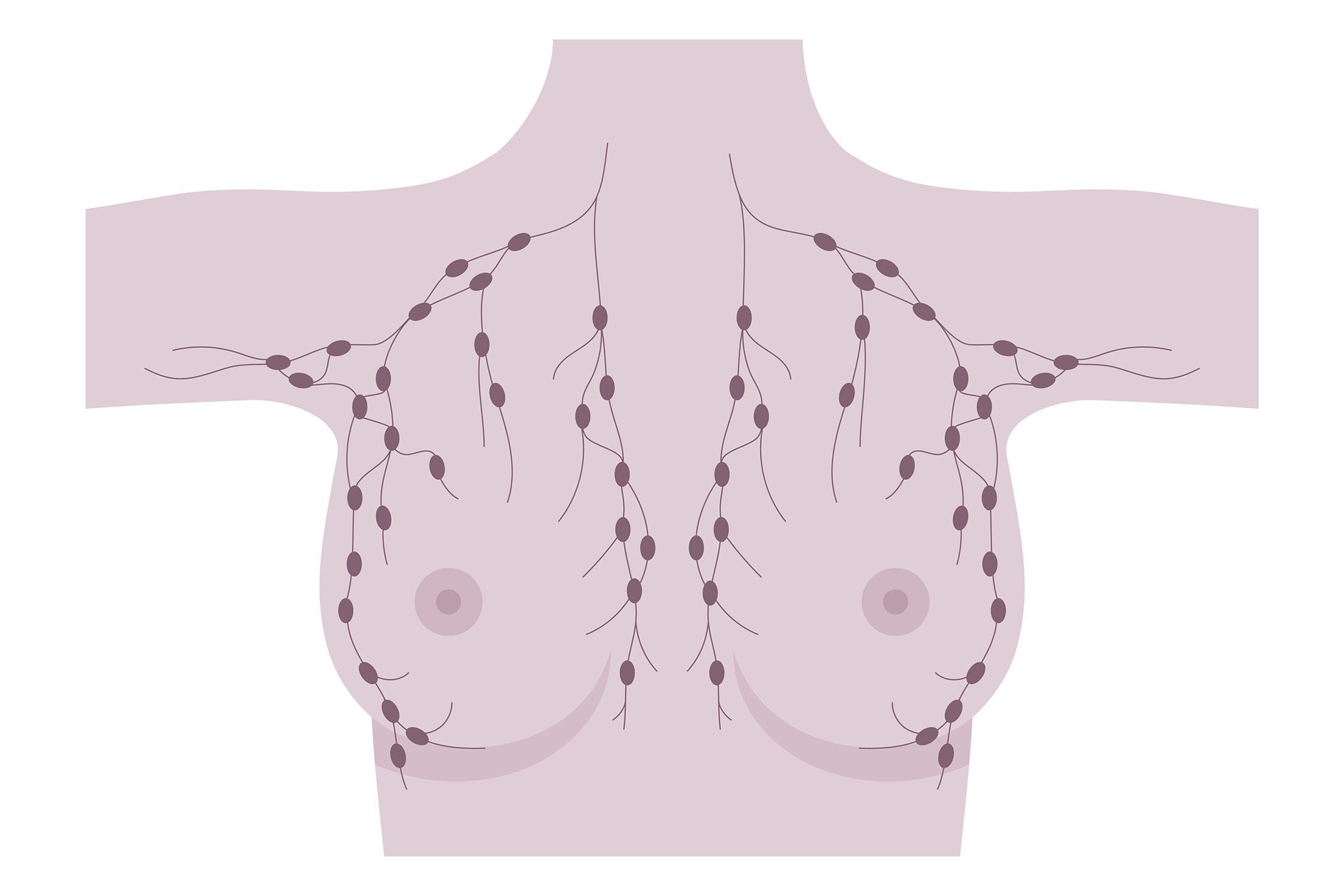
The overall estimated incidence of chronic arm edema post-breast cancer is approximately 21.4%, with a systematic review reporting an incidence rate of 17% among survivors. Chronic arm edema is often linked to the lymphatic and blood vessels within the thorax and upper limbs. Several factors heighten the risk, including axillary lymph node dissection (ALND), radiation therapy, higher body mass index (BMI), and chemotherapy. Additionally, positive lymph node status, larger tumor size, estrogen receptor-negative breast cancer, and seroma formation after surgery are significant contributors.
Understanding these risks can help in early detection and management. Effective breast cancer management includes regular monitoring of the lymphatic system to detect early signs of lymphedema. For personalized advice and treatment options, schedule an appointment with Dr. Gorman at Texas Breast Center.
How does lymphedema impact the quality of life of breast cancer survivors?
Lymphedema involves the lymphatic system and can significantly impact the quality of life of breast cancer survivors. Physically, lymphadema can cause inflammation, pain, and reduced range of motion, affecting a woman’s daily activities. Additionally, lymphedema can cause swelling in the fingers and require the use of compression bandages and garments to manage pressure. Psychologically, it can lead to depression and anxiety. As a chronic condition, lymphedema can worsen over time if not managed properly, highlighting the importance of early intervention and continuous monitoring. Recognizing the signs and understanding the need for ongoing care are crucial for maintaining the quality of life. Dr. Gorman and the team at Texas Breast Center are dedicated to providing the comprehensive support needed to manage this condition effectively.
How can lymphedema be avoided in breast cancer?
Lymphedema, a common complication following breast cancer treatment, can be managed and potentially avoided through a combination of preventive strategies, early detection, and appropriate interventions. Dr. Gorman emphasizes minimizing axillary surgery by reducing the extent of axillary lymph node dissection (ALND), as sentinel lymph node biopsy (SLNB) is less invasive and associated with a lower risk. Avoiding extensive lymphadenectomy during breast surgery can reduce the risk of damaging lymphatic vessels and lymph nodes. Preventive lymphatic surgery, such as the lymphatic microsurgical preventing healing approach (LYMPHA), performed during ALND to connect lymphatic channels to nearby veins, can also reduce the risk of lymphedema.
Wearing compression garments, such as sleeves or bras, immediately after surgery is recommended by Dr. Gorman to help prevent fluid buildup. Compression garments apply pressure to assist in lymphatic drainage. Studies have shown that early use of compression garments can reduce the incidence of lymphedema. It is crucial to have these garments properly fitted by a specialist and to wear them as recommended, especially during activities that may increase lymphatic load.
Dr. Gorman also advocates for regular, supervised exercise programs, including strength and aerobic training, to help reduce the risk of lymphedema by promoting lymphatic flow and maintaining a healthy body weight. Specific exercises targeting the arms, shoulders, and chest, such as neck rotations, shoulder rolls, and deep breathing exercises, can be particularly beneficial. Maintaining a healthy weight through diet and exercise can significantly reduce the risk of lymphedema, as obesity is a known risk factor. Incorporating lymphatic drainage massage as part of physical therapy can also support lymph flow.
Keeping the skin clean and moisturized helps avoid complications that affect the lymph glands and vessels and prevents infections that can trigger lymphedema. Dr. Gorman advises avoiding cuts, burns, and insect bites, and promptly treating any signs of infection, such as redness or swelling, to prevent the onset of lymphedema.
Early detection through regular monitoring of limb volume and other symptoms can help catch lymphedema before it becomes severe. Techniques such as bioimpedance spectroscopy (BIS) and circumferential measurements are useful for early detection. Dr. Gorman ensures that patients are educated about the signs and symptoms of lymphedema and the importance of early intervention, empowering them with knowledge about self-care strategies. A multidisciplinary team, including surgeons, physical therapists, and lymphedema specialists, provides comprehensive care and tailored prevention strategies for patients at risk of lymphedema.
While there is no guaranteed way to completely prevent lymphedema, a combination of surgical techniques, the use of compression garments, regular exercise, weight management, and vigilant skin care can significantly reduce the risk. Early detection and a proactive approach to monitoring and managing symptoms, as recommended by Dr. Gorman, are essential for improving the quality of life for breast cancer survivors.
Take Control of Lymphedema With Texas Breast Center
Lymphedema can be a challenging complication for breast cancer survivors, but with the right strategies and support, it can be managed effectively. Dr. Gorman and the team at Texas Breast Center are committed to providing the highest level of care and expertise to help you navigate this condition. By implementing preventive measures, monitoring for early signs, and maintaining a proactive approach to management, you can significantly improve your quality of life. For personalized advice and a comprehensive care plan, reach out to Texas Breast Center and take the first step towards better health.
FAQ’s About Lymphedema and Breast Cancer
When does lymphedema start after a mastectomy?
Lymphedema can start soon after a mastectomy, with axillary surgery or lymph nodes, or it may develop months or even years later. At Texas Breast Center, Dr. Gorman advises early monitoring post-surgery to catch any signs of lymphedema early, which can help manage and mitigate symptoms effectively.
What triggers lymphedema flare-ups?
Lymphedema flare-ups can be triggered by infection, injury, or overuse of the affected limb. Dr. Gorman recommends maintaining good skin care, avoiding heavy lifting, and wearing compression garments as preventive measures to minimize the risk of flare-ups.
What are the odds of lymphedema after a mastectomy?
The odds of developing lymphedema after a mastectomy with lymph node surgery vary, but studies suggest that about 20-40% of patients may experience it. Dr. Gorman emphasizes the importance of regular follow-ups and early intervention at Texas Breast Center to reduce these odds.
What are the odds of lymphedema after a lumpectomy?
The risk of lymphedema after a lumpectomy with targeted lymph node surgery is generally lower than after a surgery with more extensive lymph node surgery, typically around 5-10%. However, Dr. Gorman and the team at Texas Breast Center still recommend vigilance and proactive measures to manage this risk.
What does breast lymphedema look like?
Breast lymphedema can cause swelling, a feeling of heaviness, and skin changes such as thickening or redness. Dr. Gorman at Texas Breast Center can provide a thorough assessment and personalized care plan to manage these symptoms effectively.
How does lymphedema make you feel?
Lymphedema can cause physical discomfort, including swelling, pain, and restricted movement, as well as emotional stress. Dr. Gorman and the team at Texas Breast Center are dedicated to supporting patients both physically and emotionally through comprehensive care.
Do compression sleeves help with lymphedema after breast cancer?
Yes, compression sleeves can be very effective in managing lymphedema by promoting lymphatic drainage and reducing swelling. Dr. Gorman advises proper fitting and regular use of compression garments, particularly during activities that may increase lymphatic load.
What can I do to reduce lymphedema?
To reduce the risk of lymphedema, follow Dr. Gorman’s recommendations: maintain a healthy weight, practice good skin care, engage in regular exercise, and use compression garments as advised. Texas Breast Center offers comprehensive guidance on these preventive strategies.
What is a lymphedema drain?
A lymphedema drain is a surgical device used to remove excess fluid buildup in the affected area. Dr. Gorman can explain the procedure and benefits of using a lymphedema drain during your consultation at Texas Breast Center to manage severe cases effectively.
Does massage help lymphedema?
Manual lymphatic drainage massage can help reduce lymphedema by encouraging the flow of lymphatic fluid through lymph vessels. Dr. Gorman often includes this as part of a comprehensive breast cancer management plan at Texas Breast Center.
Can I decline to have any lymph nodes removed with breast cancer?
While some lymph node removal, or lymphadenectomy, might be necessary to prevent the spread of cancer, Dr. Gorman will evaluate the need based on your specific case to minimize impact on the lymphatic system and reduce the risk of lymphedema.

Valerie Gorman, MD, FACS, is a breast cancer surgeon. She is board certified by the American Board of Surgery and serves as Chief of Surgery and Medical Director of Surgical Services at Baylor Scott & White Medical Center – Waxahachie. She is the Clinical Assistant Professor of Medical Education position at the Texas A&M University College of Medicine.
- Certificate, Physician Leadership Program, Southern Methodist University, Dallas, Texas (2010)
- M.D., University of Texas Southwestern Medical School at Dallas, Texas (June 1999)
- B.S., Biola University, LaMirada, California, (1994) Magna Cum Laude
Major: Biochemistry - Residency in General Surgery, University of Texas Southwestern Medical Center at Dallas, Texas (June 2004)